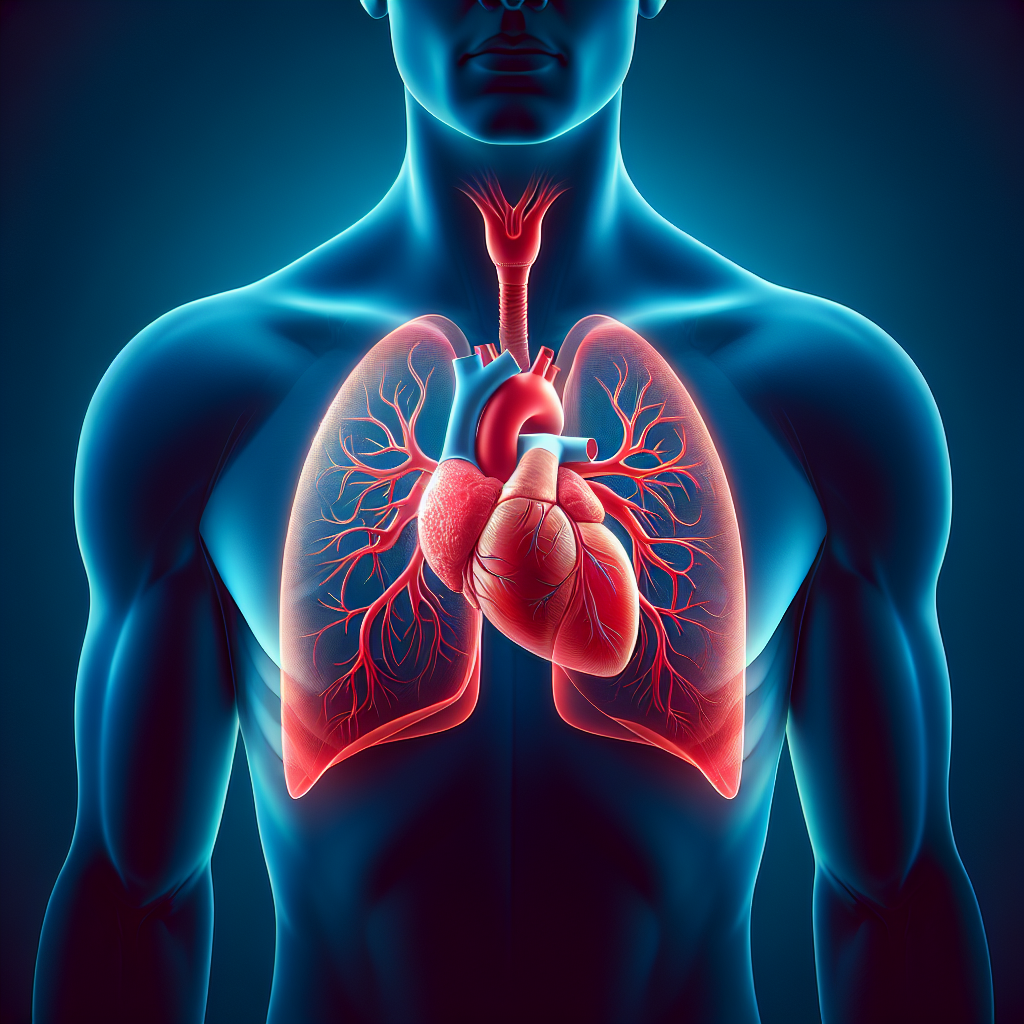
Have you ever wondered about the connection between asthma and heart disease? It turns out that these two seemingly unrelated conditions can actually be linked. Asthma, a chronic respiratory condition that affects the airways, has been found to increase the risk of developing heart disease. Research has shown that individuals with asthma are more likely to experience cardiovascular issues such as high blood pressure, heart attack, and stroke. Understanding this relationship is crucial for both asthma and heart disease management, as it highlights the importance of comprehensive care for individuals with these conditions. So, let’s explore further to uncover the intriguing connection between asthma and heart disease. Asthma and heart disease may seem like two unrelated conditions, but they actually share several risk factors, mechanisms, and impacts. Understanding the connection between asthma and heart disease is crucial for healthcare professionals and individuals who suffer from these conditions. In this article, we will explore the risk factors for asthma and heart disease, the similarities between the two, the shared mechanisms linking them, the impact each has on the other, diagnosis and treatment considerations, prevention and management strategies, the importance of coordinated care, addressing common comorbidities, and the role of patient education and self-management.
Risk Factors for Asthma and Heart Disease
Genetic Factors
Both asthma and heart disease can have a genetic component. If you have a family history of either condition, you may be at a higher risk of developing them. Certain genes and variations can make individuals more susceptible to asthma or heart disease, although the precise genetic factors are still being studied.
Environmental Factors
The environment we live in can greatly influence our risk of developing asthma and heart disease. Exposure to certain allergens, pollutants, and toxins can trigger asthma symptoms and contribute to the development of heart disease. Living in areas with high levels of air pollution, for example, has been linked to an increased risk of both conditions.
Lifestyle Factors
Your lifestyle choices can also play a significant role in the development of asthma and heart disease. Factors such as obesity, smoking, and a sedentary lifestyle are associated with an increased risk of both conditions. Maintaining a healthy weight, not smoking, and engaging in regular physical activity can help reduce your risk.
Similarities Between Asthma and Heart Disease
Chronic Inflammation
Asthma and heart disease are characterized by chronic inflammation in their respective organs. In asthma, the airways become inflamed, leading to symptoms such as wheezing and shortness of breath. In heart disease, inflammation within the blood vessels can contribute to the development of atherosclerosis, which narrows the arteries and increases the risk of heart attack and stroke.
Narrowing of Blood Vessels
Both asthma and heart disease involve a narrowing of blood vessels. In asthma, the narrowing occurs within the airways, making it difficult for air to flow in and out of the lungs. In heart disease, the narrowing occurs within the coronary arteries, restricting blood flow to the heart. This narrowing can impair the function of both the lungs and the heart.
Increased Risk of Blood Clots
Asthma and heart disease can also increase the risk of blood clots. In asthma, the inflammation and narrowing of the airways can lead to the formation of blood clots, which can further obstruct airflow. In heart disease, the narrowed blood vessels can promote the formation of blood clots, which can block blood flow to the heart and cause a heart attack.
Shared Mechanisms Linking Asthma and Heart Disease
Systemic Inflammation
In addition to the localized inflammation in their respective organs, asthma and heart disease are both associated with systemic inflammation. This means that inflammation is present throughout the body, not just in the lungs or the heart. Systemic inflammation can have far-reaching effects, contributing to various complications in both conditions.
Oxidative Stress
Oxidative stress, which occurs when there is an imbalance between free radicals and antioxidants in the body, is another shared mechanism between asthma and heart disease. Oxidative stress can damage cells and tissues, promoting inflammation and contributing to the progression of both conditions. Minimizing oxidative stress through a healthy diet and lifestyle can help mitigate the impact on both the lungs and the heart.
Immune Dysfunction
Both asthma and heart disease involve immune dysfunction. In asthma, the immune system overreacts to harmless substances, triggering an inflammatory response in the airways. In heart disease, immune cells play a role in the development and progression of atherosclerosis. Targeting immune dysfunction through medications and lifestyle interventions can be beneficial for managing both conditions.
Impact of Asthma on Heart Disease
Direct Effects on the Heart
Having asthma can directly impact the health of your heart. The chronic inflammation and oxidative stress associated with asthma can contribute to the development of heart disease. Additionally, asthma attacks, especially severe ones, can put stress on the heart and increase the risk of cardiovascular events. It is important for individuals with asthma to closely monitor their heart health and take steps to manage their asthma effectively.
Indirect Effects on Cardiovascular Health
Asthma can also have indirect effects on cardiovascular health. Medications used to manage asthma, such as beta-agonists and corticosteroids, may have side effects that can affect the heart, such as increased heart rate or blood pressure. It is essential for healthcare providers to carefully consider the cardiovascular effects of asthma medications when treating individuals with both conditions.
Impact of Heart Disease on Asthma
Reduced Lung Function
Heart disease can negatively impact lung function. When the heart is unable to pump blood effectively, fluid can accumulate in the lungs, causing shortness of breath and reducing lung function. This can make asthma symptoms worse and increase the risk of asthma attacks. Managing heart disease effectively is crucial for maintaining optimal lung function in individuals with asthma.
Increased Asthma Severity
People with heart disease may experience an exacerbation of asthma symptoms. The stress placed on the body by heart disease can trigger asthma attacks or worsen existing asthma symptoms. It is important for individuals with both conditions to work closely with their healthcare providers to manage both their heart disease and asthma effectively.
Impaired Response to Asthma Medications
Heart disease can also impact the effectiveness of asthma medications. Certain medications used to treat heart disease, such as beta blockers, can interfere with the action of asthma medications, making them less effective. It is essential for healthcare providers to consider the potential interactions between asthma and heart disease medications to ensure optimal treatment outcomes.
Diagnosis and Treatment Considerations
Effects of Asthma on Cardiac Testing
When evaluating individuals with both asthma and heart disease, healthcare providers may need to consider the potential impact of asthma on cardiac testing. Asthma symptoms, such as shortness of breath and chest tightness, can mimic heart-related symptoms, leading to uncertainty in the diagnosis. Special considerations may be required to ensure accurate testing and interpretation of results.
Effects of Heart Disease on Asthma Treatment
Heart disease can also affect the treatment of asthma. Certain asthma medications, such as beta-agonists, may need to be used with caution in individuals with underlying heart conditions. Healthcare providers need to strike a balance between managing asthma symptoms and minimizing potential cardiovascular risks when prescribing medications to individuals with both conditions.
Prevention and Management Strategies
Cardiovascular Risk Reduction in Asthmatic Patients
To reduce the risk of heart disease in individuals with asthma, it is essential to focus on cardiovascular risk reduction strategies. This includes promoting a healthy lifestyle, such as eating a balanced diet, engaging in regular physical activity, maintaining a healthy weight, and avoiding smoking. Additionally, managing asthma effectively to minimize chronic inflammation and oxidative stress can also help reduce cardiovascular risks.
Asthma Management in Individuals with Heart Disease
Individuals with heart disease can benefit from proper asthma management to reduce the impact of asthma on their cardiovascular health. This includes taking prescribed asthma medications as directed, avoiding triggers that exacerbate asthma symptoms, and seeking prompt treatment for asthma attacks. Collaborative care between cardiologists and pulmonologists is crucial for managing both conditions effectively.
Coordinated Care Approach
Collaboration Between Cardiologists and Pulmonologists
Coordinated care between cardiologists and pulmonologists is essential for individuals with both asthma and heart disease. A collaborative approach ensures that both conditions are effectively managed without compromising the health of the individual. Close communication and shared decision-making between healthcare providers can result in better treatment outcomes and improved quality of life.
Pharmacotherapy Considerations
When treating individuals with both asthma and heart disease, pharmacotherapy considerations are necessary to avoid potential interactions and adverse effects. This includes selecting asthma medications that are safe for individuals with underlying heart conditions and carefully considering the cardiovascular effects of heart disease medications. Dose adjustments or the use of alternative medications may be required to optimize therapeutic outcomes.
Addressing Common Comorbidities
Obesity
Obesity is a common comorbidity in individuals with both asthma and heart disease. Excess weight can worsen asthma symptoms and increase the risk of heart disease. Addressing obesity through lifestyle modifications, such as adopting a healthy diet and engaging in regular physical activity, can have significant benefits for both conditions.
Smoking
Smoking is a major risk factor for both asthma and heart disease. It can trigger asthma attacks, worsen heart disease, and increase the risk of developing both conditions. Encouraging smoking cessation through counseling and support services is crucial for individuals with asthma and heart disease to improve their overall health outcomes.
Depression
Depression is another common comorbidity in individuals with asthma and heart disease. The emotional toll of living with these chronic conditions can lead to feelings of sadness, hopelessness, and decreased motivation to engage in self-care. Identifying and addressing depression through appropriate psychological support can help individuals better manage their asthma and heart disease.
Role of Patient Education and Self-Management
Promoting Healthy Lifestyle Choices
Patient education plays a vital role in the management of both asthma and heart disease. Providing information about the relationship between the two conditions and promoting healthy lifestyle choices can empower individuals to take control of their health. Educating patients on proper nutrition, regular physical activity, smoking cessation, and stress management can have a profound impact on their overall well-being.
Recognizing Symptoms and Seeking Prompt Treatment
For individuals with both asthma and heart disease, recognizing symptoms and seeking prompt treatment is essential. It is crucial for patients to understand the warning signs of both conditions and to seek medical attention when necessary. Encouraging self-monitoring and providing action plans for managing exacerbations can empower individuals to effectively manage both asthma and heart disease.
In conclusion, asthma and heart disease are not isolated conditions but are interconnected through shared risk factors, mechanisms, and impacts. Recognizing and understanding this relationship is crucial for healthcare professionals and individuals dealing with these conditions. By addressing common risk factors, managing chronic inflammation and oxidative stress, promoting a healthy lifestyle, and providing coordinated care, we can improve the overall outcomes for individuals with asthma and heart disease. With proper education, self-management, and support, individuals can lead fulfilling lives while effectively managing both conditions.