When you have asthma, your airways become inflamed and narrow, making it difficult to breathe. This can lead to symptoms such as wheezing, coughing, chest tightness, and shortness of breath. Asthma attacks can be triggered by allergens, exercise, stress, or respiratory infections. It’s important to seek proper treatment and management strategies to keep your asthma under control and lead a healthy, active lifestyle. Understanding how asthma affects your body can help you better manage your condition and improve your quality of life. What Happens To Your Body When You Have Asthma?
Have you ever wondered what exactly is happening inside your body when you struggle to breathe due to asthma? Understanding how asthma affects your body can help you better manage your condition and improve your quality of life. Let’s take a closer look at what happens to your body when you have asthma.
What is Asthma?
Asthma is a chronic respiratory condition that affects the airways in the lungs. People with asthma have sensitive airways that react to triggers such as allergens, smoke, cold air, exercise, and stress. When these triggers cause the airways to become inflamed, they become narrower, making it harder to breathe.
When you have asthma, your body’s immune system overreacts to certain triggers, causing inflammation and swelling in the airways. This leads to symptoms such as wheezing, coughing, chest tightness, and shortness of breath. Understanding the underlying mechanisms of asthma can help you better manage your symptoms and prevent asthma attacks.
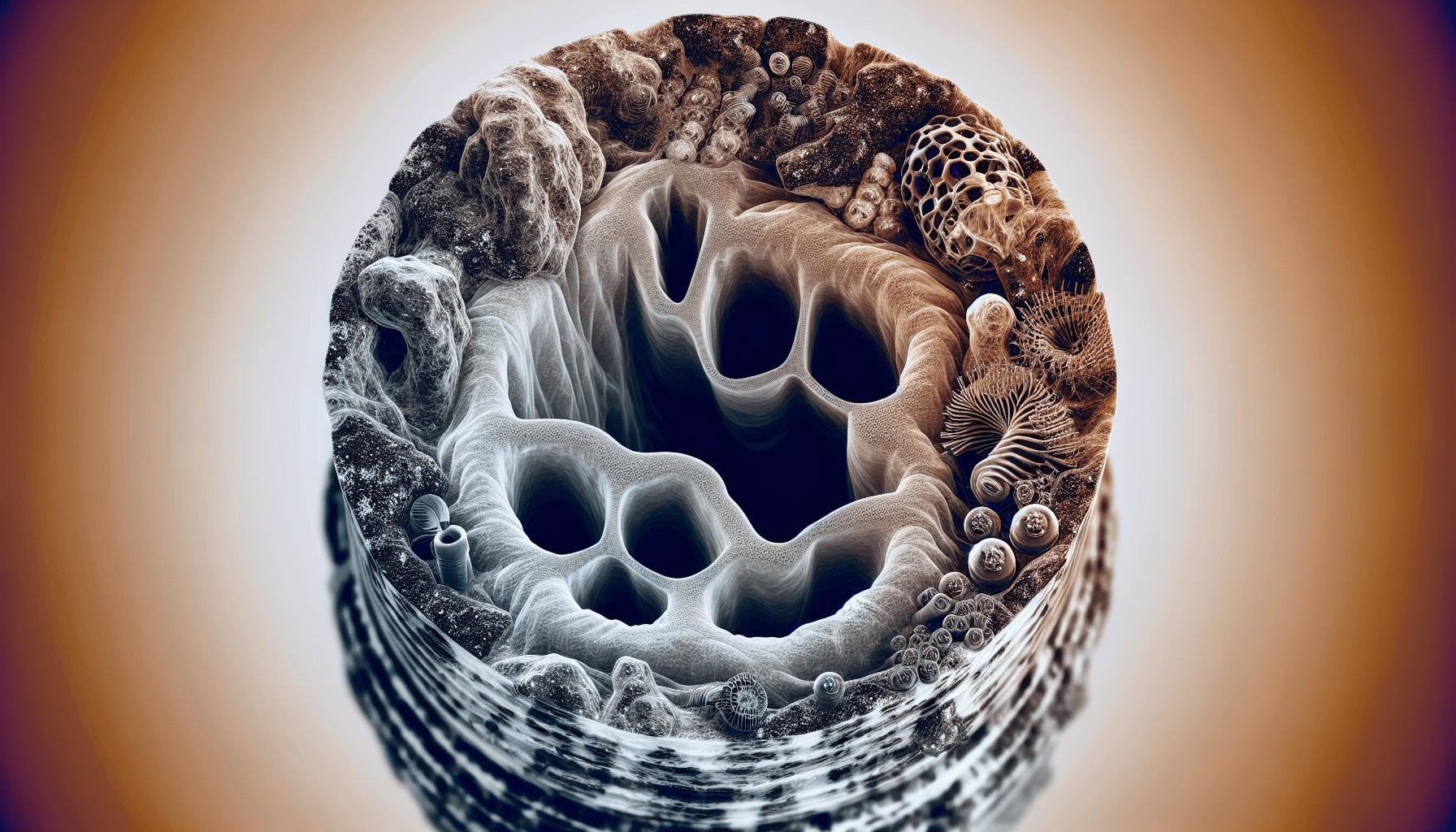
Inflammation in the Airway
The first step in understanding what happens to your body when you have asthma is to look at the role of inflammation in the airways. In people with asthma, the immune system mistakenly identifies harmless substances such as pollen, dust mites, pet dander, or mold as harmful invaders. This triggers an immune response that leads to inflammation in the airways.
The inflammation in the airways causes them to become swollen and produce excess mucus, making it difficult for air to flow freely. This can result in difficulty breathing, wheezing, coughing, and chest tightness. By reducing inflammation in the airways, asthma symptoms can be better controlled.
Airway Constriction
One of the hallmark features of asthma is airway constriction, also known as bronchoconstriction. When the airways become inflamed, the muscles around them tighten, causing a narrowing of the airways. This makes it harder for air to pass through, leading to symptoms such as wheezing and shortness of breath.
Bronchoconstriction is a key factor in asthma attacks, which can be triggered by various factors such as allergens, respiratory infections, exercise, or stress. By understanding how airway constriction affects your breathing, you can take steps to prevent asthma attacks and manage your symptoms more effectively.
Common Triggers of Asthma
Understanding the triggers that can worsen your asthma symptoms is essential for managing your condition. By identifying and avoiding these triggers, you can reduce the frequency and severity of asthma attacks. Here are some common triggers of asthma:
Allergens
Allergens such as pollen, dust mites, pet dander, and mold spores can trigger asthma symptoms in people with allergic asthma. When these allergens come into contact with the airways, they can cause inflammation and bronchoconstriction, leading to breathing difficulties.
If you have allergic asthma, it’s important to identify your specific triggers and take steps to minimize your exposure to them. This may include using air purifiers, regularly cleaning your home, and avoiding outdoor activities during high pollen seasons.
Smoke and Air Pollution
Exposure to tobacco smoke, secondhand smoke, and air pollution can worsen asthma symptoms and increase the risk of asthma attacks. The chemicals in smoke and pollution can irritate the airways, leading to inflammation and bronchoconstriction.
If you have asthma, it’s important to avoid smoking and exposure to secondhand smoke. You should also be mindful of air quality and take precautions on days when air pollution levels are high. By protecting your lungs from smoke and pollution, you can reduce the risk of asthma exacerbations.
Respiratory Infections
Respiratory infections such as the common cold, flu, and sinus infections can trigger asthma attacks in some people. Infections can cause inflammation in the airways and make it harder to breathe, especially in individuals with asthma.
If you have asthma, it’s important to take steps to prevent respiratory infections, such as practicing good hand hygiene, getting vaccinated, and avoiding close contact with sick individuals. By reducing your risk of infections, you can help prevent asthma exacerbations.
Symptoms of Asthma
Recognizing the symptoms of asthma is essential for managing your condition and seeking timely medical treatment. Asthma symptoms can vary from person to person and may range from mild to severe. Here are some common symptoms of asthma:
Wheezing
Wheezing is a high-pitched whistling sound that occurs when air flows through narrowed airways. It is a hallmark symptom of asthma and is often heard during exhalation. Wheezing can be a sign of bronchoconstriction and inflammation in the airways.
If you experience wheezing, it’s important to seek medical attention to determine the underlying cause and receive appropriate treatment. Your healthcare provider may recommend medications to help open up your airways and reduce inflammation.
Coughing
Coughing is another common symptom of asthma, especially during the night or early morning. Coughing may be dry or produce mucus and can be triggered by allergens, exercise, cold air, or respiratory infections. Persistent coughing can be a sign of poorly controlled asthma.
If you have a chronic cough that is not improving, it’s important to see your healthcare provider for a proper evaluation. Your provider may recommend asthma medications or other treatments to help manage your symptoms and improve your quality of life.
Chest Tightness
Chest tightness is a sensation of pressure or squeezing in the chest that can occur during asthma attacks. It may feel like someone is sitting on your chest or like you are wearing a tight belt around your chest. Chest tightness is often accompanied by difficulty breathing and wheezing.
If you experience chest tightness, it’s important to seek medical attention as soon as possible. Chest tightness can be a sign of a severe asthma attack that requires immediate treatment. Your healthcare provider can help determine the best course of action to relieve your symptoms and prevent complications.
Shortness of Breath
Shortness of breath, also known as dyspnea, is a common symptom of asthma that can be frightening and uncomfortable. It may feel like you can’t get enough air into your lungs or like you are suffocating. Shortness of breath can occur during physical exertion, at rest, or during asthma attacks.
If you experience sudden or severe shortness of breath, it’s important to seek emergency medical care. Shortness of breath can be a sign of a life-threatening asthma attack that requires immediate intervention. Your healthcare provider can help assess your condition and provide the necessary treatment to improve your breathing.
Diagnosis of Asthma
Diagnosing asthma involves a combination of medical history, physical examination, and lung function tests. Your healthcare provider will ask about your symptoms, triggers, and family history of asthma to determine if you have asthma. Here are some common tests used to diagnose asthma:
Spirometry
Spirometry is a lung function test that measures how much air you can breathe in and out of your lungs. It assesses your lung capacity, airflow, and how well your lungs are functioning. Spirometry can help determine if you have asthma and how well your asthma is controlled.
During a spirometry test, you will be asked to inhale deeply and then exhale forcefully into a tube connected to a spirometer. The test results will show your lung function parameters, such as forced vital capacity (FVC) and forced expiratory volume in one second (FEV1). Abnormal results may indicate asthma or other lung conditions.
Peak Flow Measurement
Peak flow measurement is a simple test that measures how fast you can blow air out of your lungs. It assesses how well your airways are functioning and can help monitor your asthma symptoms. Peak flow measurements can be used to track changes in your lung function and evaluate the effectiveness of your asthma treatment.
To perform a peak flow measurement, you will use a peak flow meter to blow air into a mouthpiece and record the highest flow rate achieved. You will need to measure your peak flow regularly and keep a log of the results. Changes in peak flow readings may indicate worsening asthma symptoms or the need for an adjustment in your treatment plan.
Allergy Testing
Allergy testing may be recommended to identify specific triggers that worsen your asthma symptoms. Skin prick tests or blood tests can help determine if you have allergies to common substances such as pollen, dust mites, pet dander, or mold. Avoiding allergens can reduce inflammation in your airways and improve your asthma control.
If you have allergic asthma, allergy testing can help you identify your specific triggers and take steps to minimize your exposure to them. Your healthcare provider may recommend allergy medications, immunotherapy, or environmental control measures to help manage your allergies and asthma.
Treatment of Asthma
Managing asthma involves a combination of medications, lifestyle modifications, and self-care strategies. By working closely with your healthcare provider, you can develop a personalized treatment plan that meets your needs and helps control your asthma symptoms. Here are some common treatments for asthma:
Bronchodilators
Bronchodilators are medications that help open up the airways and relieve bronchoconstriction in asthma. Short-acting bronchodilators such as albuterol are used as rescue inhalers to provide quick relief of asthma symptoms. Long-acting bronchodilators may be used to control persistent asthma symptoms.
Bronchodilators work by relaxing the muscles around the airways and improving airflow into the lungs. They are typically inhaled through a metered-dose inhaler or nebulizer for quick absorption into the lungs. By using bronchodilators as prescribed, you can alleviate bronchoconstriction and improve your breathing.
Inhaled Corticosteroids
Inhaled corticosteroids are anti-inflammatory medications that help reduce inflammation in the airways and prevent asthma symptoms. They are commonly used as maintenance therapy to control persistent asthma and prevent asthma attacks. Inhaled corticosteroids are effective in reducing airway inflammation and improving lung function.
By using inhaled corticosteroids regularly as prescribed, you can reduce the frequency and severity of asthma attacks. These medications are typically inhaled through a metered-dose inhaler or dry powder inhaler to deliver the medication directly to the airways. It’s important to use inhaled corticosteroids consistently to maintain asthma control.
Leukotriene Modifiers
Leukotriene modifiers are medications that help block the action of leukotrienes, chemicals that contribute to inflammation in the airways. They are used to control asthma symptoms and reduce airway inflammation in people with allergic asthma. Leukotriene modifiers may be taken orally in pill form or as a chewable tablet.
By taking leukotriene modifiers as prescribed, you can help prevent asthma symptoms and improve your lung function. These medications are typically used in combination with other asthma treatments to achieve better asthma control. It’s important to follow your healthcare provider’s recommendations for using leukotriene modifiers.
Allergy Immunotherapy
Allergy immunotherapy, also known as allergy shots or sublingual immunotherapy, is a treatment option for people with allergic asthma. It involves receiving injections or oral doses of allergens to desensitize the immune system and reduce allergic reactions. Allergy immunotherapy can help reduce asthma symptoms and improve quality of life.
If you have allergic asthma, allergy immunotherapy may be recommended to help reduce your sensitivity to specific allergens. This treatment can be effective in reducing inflammation in the airways and preventing asthma attacks triggered by allergens. Your healthcare provider can help determine if allergy immunotherapy is a suitable option for you.
Prevention of Asthma Attacks
Preventing asthma attacks involves identifying triggers, managing symptoms, and taking proactive steps to protect your lungs. By following an asthma action plan and working closely with your healthcare provider, you can reduce the risk of asthma attacks and maintain good asthma control. Here are some tips for preventing asthma attacks:
Identify Triggers
Identifying and avoiding asthma triggers is essential for preventing asthma attacks. Common triggers such as allergens, smoke, pollution, and respiratory infections can worsen your asthma symptoms. By keeping track of your triggers and taking steps to minimize your exposure to them, you can reduce the frequency and severity of asthma attacks.
Follow Your Treatment Plan
Adhering to your asthma treatment plan is crucial for managing your symptoms and preventing asthma attacks. Take your medications as prescribed, monitor your lung function regularly, and track changes in your symptoms. By working closely with your healthcare provider, you can develop a personalized treatment plan that meets your needs and improves your asthma control.
Use Your Inhaler Correctly
Using your inhaler correctly is important for ensuring that your medications reach the airways and provide effective relief. Follow the instructions provided by your healthcare provider on how to use your inhaler properly. This may involve coordinating your breath with pressing the inhaler, inhaling deeply, and holding your breath for a few seconds.
Stay Active
Regular physical activity can help improve lung function, strengthen respiratory muscles, and reduce the risk of asthma attacks. Engage in activities such as walking, biking, swimming, or yoga to stay active and maintain good lung health. Consult your healthcare provider before starting an exercise program to ensure it is safe for your asthma.
Monitor Your Symptoms
Keeping track of your asthma symptoms and peak flow measurements can help you identify patterns and triggers that exacerbate your asthma. Use a peak flow meter to measure your lung function regularly and record the results in a diary. Share this information with your healthcare provider to help monitor your asthma control and adjust your treatment plan as needed.
Seek Medical Help
If you experience worsening asthma symptoms, severe shortness of breath, or an asthma attack that does not improve with rescue medications, seek emergency medical care immediately. Asthma attacks can be life-threatening and require prompt intervention to prevent complications. Your healthcare provider can help assess your condition and provide the necessary treatment to improve your breathing.
By following these tips and working closely with your healthcare provider, you can reduce the risk of asthma attacks and maintain good asthma control. Remember that asthma is a manageable condition, and with proper treatment and self-care, you can lead a healthy and active life. If you have any questions or concerns about your asthma, don’t hesitate to reach out to your healthcare provider for guidance and support. Together, you can develop a comprehensive asthma management plan that meets your needs and improves your quality of life.