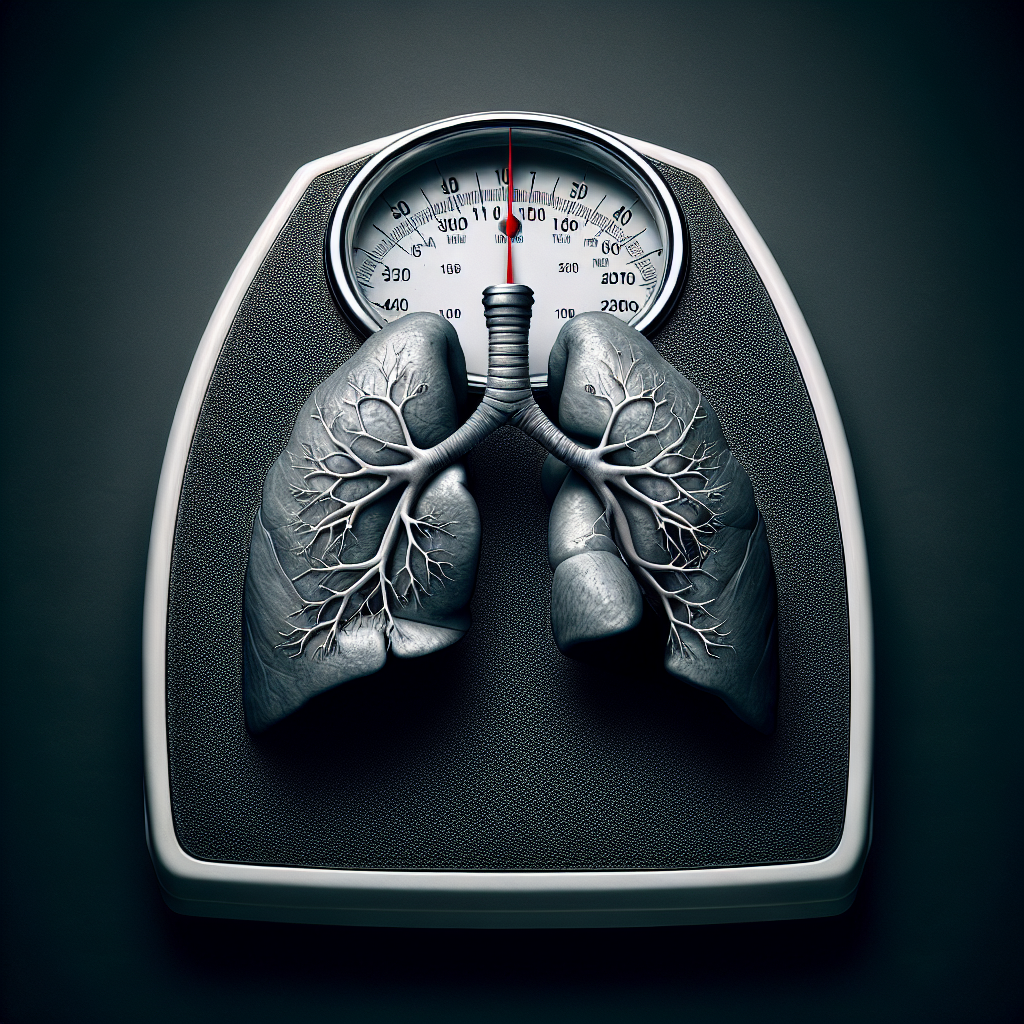
Have you ever wondered about the connection between obesity and asthma? It’s a topic that has sparked considerable interest among researchers and healthcare professionals alike. In this article, we will explore the correlation between these two prevalent health issues and shed light on how they can impact each other. So, if you’re curious to learn more about the relationship between obesity and asthma, read on to discover the fascinating insights behind this complex interaction.
Understanding Obesity
Definition of obesity
Obesity is a medical condition characterized by excessive accumulation of body fat, to the extent that it may have adverse effects on a person’s health. It is typically determined by calculating the body mass index (BMI), which takes into account both weight and height.
Factors contributing to obesity
There are various factors that contribute to the development of obesity. These include genetics, lifestyle choices, environmental factors, and socioeconomic status. Genetic predisposition can influence a person’s susceptibility to obesity, and certain genes may affect appetite regulation and metabolism. Additionally, a sedentary lifestyle, poor dietary choices, and high-calorie intake can contribute to weight gain. Environmental factors such as the availability of unhealthy food options and limited opportunities for physical activity also play a significant role. Furthermore, socioeconomic factors, such as income and education level, can impact access to healthy food and resources for maintaining a healthy lifestyle.
Prevalence of obesity
Obesity has become a growing concern worldwide, with its prevalence steadily increasing over the years. In many developed countries, obesity rates have reached epidemic proportions. According to the World Health Organization (WHO), in 2016, more than 1.9 billion adults worldwide were overweight, and over 650 million were obese. These numbers are alarming and emphasize the urgent need for effective prevention and management strategies.
Understanding Asthma
Definition of asthma
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, shortness of breath, chest tightness, and coughing. These symptoms are often triggered by various environmental factors, including allergens, irritants, exercise, and infections.
Causes of asthma
The exact cause of asthma is still not fully understood. It is considered a complex disease resulting from a combination of genetic and environmental factors. People with a family history of asthma are more likely to develop the condition. Additionally, exposure to certain allergens, such as dust mites, pollen, or pet dander, can trigger asthma symptoms. Other non-allergic triggers, including respiratory infections, air pollutants, and occupational exposures, can also contribute to the development and exacerbation of asthma.
Prevalence of asthma
Asthma affects a significant number of individuals worldwide, with varying prevalence rates across different countries and age groups. According to the Global Asthma Report 2018, an estimated 339 million people globally had asthma in 2016. It is more prevalent in children, with approximately 11% of children worldwide and around 8.3% of adults affected by the condition. The burden of asthma is substantial, resulting in significant healthcare utilization, impaired quality of life, and even mortality in severe cases.
Obesity as a Risk Factor for Asthma
Correlation between obesity and asthma
There is a well-documented correlation between obesity and asthma, with numerous studies highlighting the increased risk of developing asthma in individuals who are overweight or obese. The exact nature of this relationship is complex and multifactorial, involving a combination of shared risk factors, biological mechanisms, and lifestyle factors.
Mechanisms linking obesity and asthma
Several biological mechanisms have been proposed to explain the link between obesity and asthma. One key factor is systemic inflammation and immune dysregulation. Adipose tissue in obese individuals releases pro-inflammatory cytokines that can contribute to airway inflammation and asthma symptoms. Additionally, the mechanical effects of excess fat can impact respiratory mechanics and lung function, leading to increased airway resistance and decreased lung volumes. The secretion of adipokines, hormones produced by adipose tissue, may also play a role in the development and exacerbation of asthma.
Impact of obesity on asthma severity
Obesity has been shown to have a significant impact on the severity and control of asthma. Studies have consistently demonstrated that obese individuals with asthma experience more frequent asthma exacerbations, reduced lung function, and decreased response to standard asthma medications. Obesity-related changes in airway inflammation, lung mechanics, and hormonal imbalances may contribute to these adverse outcomes. The burden of asthma-related symptoms can also be greater in obese individuals, affecting their quality of life and overall well-being.
Biological Mechanisms
Systemic inflammation and immune dysregulation
Obesity is associated with a chronic low-grade inflammatory state in the body, whereby adipose tissue secretes pro-inflammatory cytokines and chemokines. These circulating inflammatory mediators can reach the airways and contribute to airway inflammation, increasing the risk of asthma development or exacerbation.
Respiratory mechanics and lung function
Excess fat accumulation in the abdominal and thoracic regions can mechanically affect lung function. Increased fat around the chest wall and abdomen can restrict diaphragmatic movement and reduce lung volumes. This can lead to increased airway resistance and decreased expiratory airflow, making it more challenging for individuals with asthma to breathe.
Adipokines and their role in asthma
Adipokines are hormones secreted by adipose tissue and are involved in various physiological processes, including inflammation and metabolism. It has been suggested that adipokines, such as leptin and adiponectin, may play a role in the pathogenesis of asthma. Leptin, for example, has pro-inflammatory properties and has been associated with airway hyperresponsiveness and asthma severity. Adiponectin, on the other hand, has anti-inflammatory effects and may have a protective role against asthma development and progression.
Shared Risk Factors
Genetic predisposition
Both obesity and asthma have a genetic component, and certain genes may increase the risk of developing either condition. Specific gene variants related to appetite regulation, energy metabolism, and immune function have been implicated in the development of obesity and asthma. However, the interplay between these genetic factors and environmental influences is complex and requires further research to fully understand.
Environmental exposures
Certain environmental factors can contribute to the development of both obesity and asthma. For example, exposure to high-calorie, low-nutrient foods and drinks, as well as sedentary behaviors, can promote weight gain and the development of obesity. Similarly, exposure to allergens, air pollutants, and other respiratory irritants can trigger asthma symptoms and exacerbations. Additionally, environmental factors such as socioeconomic status and living conditions can impact access to healthy food options, healthcare, and resources for managing both conditions.
Socioeconomic factors
Socioeconomic factors, including income level, education, and access to healthcare, play a significant role in the development and management of both obesity and asthma. Limited resources, food insecurity, and lack of education about healthy lifestyle behaviors can contribute to higher obesity rates in economically disadvantaged populations. Similarly, inadequate access to healthcare and preventive measures can lead to suboptimal asthma control and outcomes in underserved communities.
Obesity and Asthma in Children
Prevalence of obesity and asthma in children
The prevalence of both obesity and asthma in children has been steadily rising over the past few decades. In many developed countries, childhood obesity rates have reached alarming levels, with around 18% of children aged 5-19 years being overweight or obese. Simultaneously, asthma remains one of the most common chronic conditions in childhood, affecting approximately 11% of children globally.
Long-term consequences
Obesity and asthma in childhood can have long-term consequences for an individual’s health and well-being. Children with obesity and asthma are at a higher risk of experiencing persistent asthma symptoms, reduced lung function, and increased asthma severity. They are also more likely to develop other obesity-related comorbidities, such as Type 2 diabetes and cardiovascular diseases, later in life.
Management strategies
Managing obesity and asthma in children requires a comprehensive approach that includes lifestyle modifications, behavioral interventions, and appropriate medical treatments. Encouraging regular physical activity, promoting a healthy diet, and addressing any underlying psychological factors are essential components of managing both conditions. In addition, asthma-specific interventions, such as appropriate use of inhaler medications and allergen avoidance, are necessary for effective asthma control.
Obesity and Asthma in Adults
Prevalence of obesity and asthma in adults
Obesity and asthma also commonly coexist in adults, with significant implications for disease management and quality of life. The prevalence of obesity in adults varies across countries, but it is consistently higher than in children. In the United States, for example, more than 40% of adults are classified as obese. Asthma, although more prevalent in childhood, can persist into adulthood, with an estimated 8.3% of adults worldwide affected.
Impact on asthma control and quality of life
Obesity can significantly impact asthma control and exacerbate symptoms in adults. Research has shown that obese adults with asthma are more likely to experience poor asthma control, increased medication use, and higher rates of hospitalizations and emergency department visits compared to their non-obese counterparts. The additional burden of obesity-related comorbidities, such as sleep apnea and gastroesophageal reflux disease, can further complicate asthma management and adversely affect overall quality of life.
Interventions for obese asthmatics
Managing asthma in obese adults requires a comprehensive approach that addresses both obesity and asthma control simultaneously. Weight loss interventions, such as dietary modifications and increased physical activity, are crucial for achieving sustainable weight loss and reducing the impact of obesity on asthma. Asthma-specific interventions, including appropriate use of inhaler medications and regular monitoring of symptoms and lung function, are also essential for effective asthma management.
Diagnosis and Assessment of Obesity-Related Asthma
Clinical evaluation
Diagnosing obesity-related asthma involves a thorough clinical evaluation by a healthcare professional. This includes obtaining a detailed medical history, assessing asthma symptoms and severity, evaluating potential risk factors, and identifying any obesity-related comorbidities. A comprehensive understanding of an individual’s overall health status is crucial for guiding appropriate management strategies.
Physical examination findings
During a physical examination, healthcare providers look for specific findings that may support a diagnosis of obesity-related asthma. These findings may include signs of increased fat distribution in the abdominal and thoracic regions, decreased lung volumes, and increased respiratory effort. Additionally, evaluating for any obesity-related comorbidities, such as hypertension or obstructive sleep apnea, can provide further insights into the impact of obesity on an individual’s health.
Diagnostic tests and measurements
Diagnostic tests and measurements play a crucial role in assessing the severity of asthma and its relationship to obesity. These may include pulmonary function tests, such as spirometry and peak flow measurements, to evaluate lung function and airway obstruction. In some cases, additional tests, such as bronchial provocation tests, may be necessary to confirm asthma diagnosis or assess asthma severity. Additionally, measures of body composition, such as BMI and waist circumference, can provide important information about an individual’s obesity status.
Management Strategies
Weight loss interventions
Weight loss interventions are a cornerstone of managing obesity-related asthma. These interventions aim to achieve sustainable weight loss through a combination of dietary modifications, increased physical activity, and behavioral changes. Encouraging a balanced diet, portion control, and reducing calorie intake can help individuals achieve and maintain a healthy weight. Regular physical activity, tailored to an individual’s abilities and preferences, is also important for promoting weight loss and overall well-being.
Asthma management strategies
Effective asthma management strategies are equally important in controlling asthma symptoms and reducing the impact of obesity on asthma. This includes the appropriate use of asthma medications, such as inhaled corticosteroids and bronchodilators, as prescribed by healthcare providers. Regular monitoring of symptoms, peak flow measurements, and periodic follow-up visits are essential for optimizing asthma control and adjusting treatment plans as needed. In some cases, allergen avoidance, pulmonary rehabilitation, and self-management education may be recommended.
Integrated care approaches
To address the complex interplay between obesity and asthma, an integrated care approach that combines weight management and asthma management is necessary. This involves coordinated efforts between healthcare providers specializing in both obesity and asthma, focusing on individualized care plans that target both conditions simultaneously. Coordination of care, effective communication, and close monitoring of progress are critical for ensuring optimal outcomes in individuals with obesity-related asthma.
Future Directions
Research gaps
While significant progress has been made in understanding the correlation between obesity and asthma, there are still several research gaps that need to be addressed. Further research is needed to unravel the underlying biological mechanisms linking obesity and asthma, as well as the influence of genetic and environmental factors. Additionally, more studies are needed to develop and evaluate targeted interventions for managing obesity-related asthma and reducing the burden of these conditions on individuals and healthcare systems.
Prevention and early intervention
Prevention and early intervention strategies hold promise in mitigating the impact of obesity and asthma on individuals’ health. Promoting healthy lifestyle behaviors from an early age, including healthy eating habits and regular physical activity, can help prevent the development of obesity and asthma in children. Early identification of at-risk individuals and timely interventions can reduce the risk of long-term complications and improve prognosis.
Potential therapeutic targets
Identifying potential therapeutic targets related to the biological mechanisms of obesity-related asthma may pave the way for novel treatment options. Targeting systemic inflammation, immune dysregulation, and adipokines could potentially reduce airway inflammation and improve asthma outcomes in obese individuals. Further research in these areas may uncover new therapeutic approaches and enhance our ability to manage obesity-related asthma effectively.
In conclusion, the correlation between obesity and asthma is well-established, with multiple factors contributing to this relationship. Biological mechanisms, shared risk factors, and lifestyle factors all play a role in the development and severity of obesity-related asthma. Understanding these factors and their interplay is crucial for devising effective prevention and management strategies. By addressing both obesity and asthma simultaneously, healthcare providers can improve outcomes and enhance the quality of life for individuals with these coexisting conditions. As research continues to uncover new insights, the future holds promise for more targeted interventions and improved management of obesity-related asthma.