Do you often find yourself struggling to distinguish between asthma and other respiratory conditions? It can be quite a challenge, especially when the symptoms may overlap. In this article, we will explore some key factors that can help you differentiate between asthma and other respiratory conditions. By understanding these differences, you will be better equipped to identify the underlying cause of your respiratory symptoms and seek appropriate medical treatment. So, let’s dive in and unravel the mysteries of asthma and other respiratory conditions together!
Asthma and its Symptoms
Definition of asthma
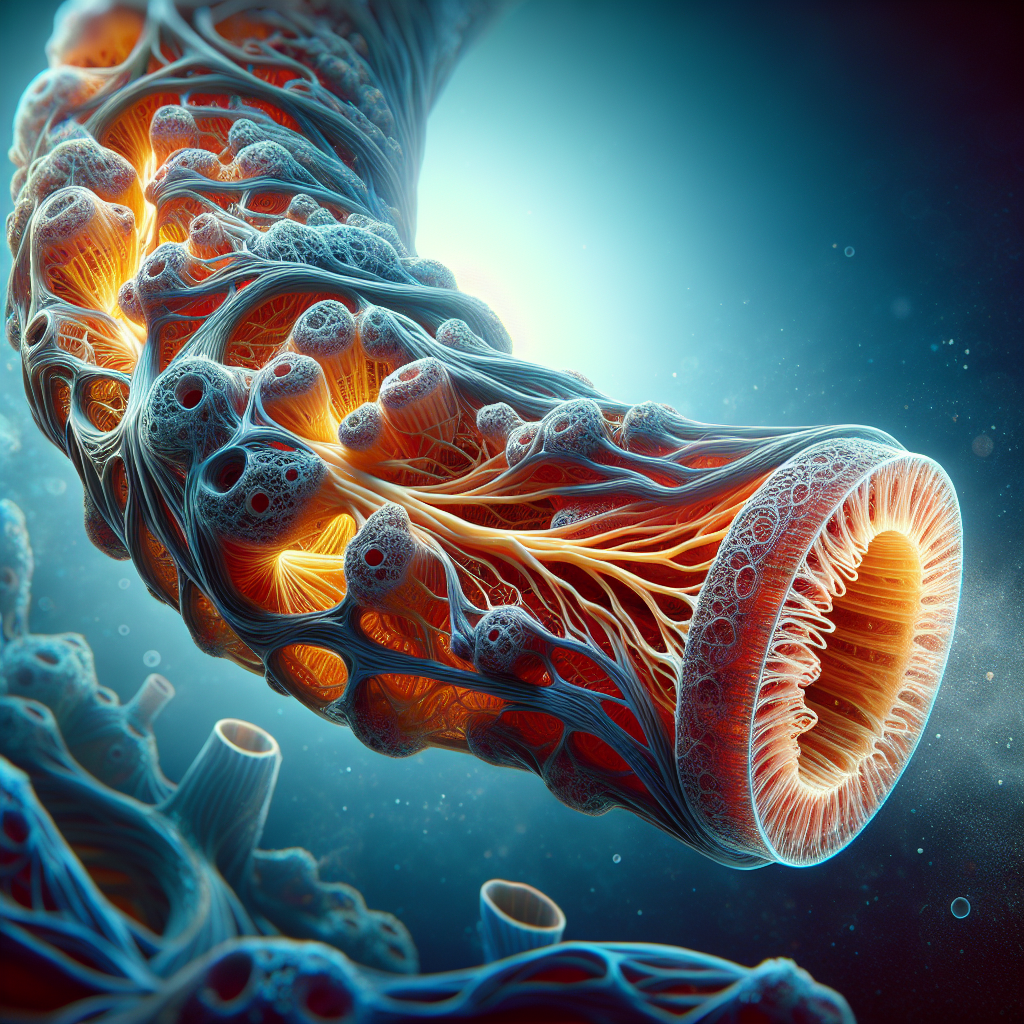
Asthma is a chronic respiratory condition that affects the airways, causing inflammation and narrowing of the bronchial tubes. This inflammation and constriction make it difficult for air to pass through, resulting in symptoms such as wheezing, shortness of breath, and coughing. Asthma is usually triggered by certain environmental factors or allergens, and it can vary in severity from person to person.
Common symptoms of asthma
The symptoms of asthma can differ from person to person, but some common signs to look out for include:
- Wheezing: A whistling sound when breathing, usually more prominent during exhaling.
- Shortness of breath: Feeling tightness in the chest and being unable to take deep breaths.
- Coughing: A persistent, dry cough that may worsen at night or with physical activity.
- Chest tightness: A sensation of pressure or tightness in the chest.
- Difficulty sleeping: Asthma symptoms may worsen at night, leading to sleep disturbances.
It’s important to note that not everyone with asthma will experience all of these symptoms, and their severity can vary. If you suspect you may have asthma, it’s crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Respiratory Conditions That Can Be Confused with Asthma
Bronchitis
Bronchitis is a respiratory condition characterized by inflammation of the bronchial tubes, which carry air to and from the lungs. While asthma and bronchitis share some symptoms, such as coughing and wheezing, there are key differences. Bronchitis is often caused by an infection, such as a cold or flu virus, and the symptoms typically include a productive cough with phlegm and a low-grade fever.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a term used to describe a group of chronic lung diseases, including chronic bronchitis and emphysema. Like asthma, COPD can cause coughing, wheezing, and shortness of breath, but it is usually associated with long-term exposure to harmful substances such as cigarette smoke. COPD symptoms tend to worsen over time and can greatly impact lung function.
Pneumonia
Pneumonia is an infection that targets the lung tissue, causing inflammation and fluid buildup. While asthma and pneumonia can present with coughing, chest discomfort, and difficulty breathing, pneumonia is usually associated with high fever, chills, and fatigue. It requires immediate medical attention as it can be severe and even life-threatening.
Allergic Rhinitis or Hay Fever
Allergic rhinitis, commonly known as hay fever, is an allergic reaction that leads to inflammation of the nasal passages. Although it primarily affects the nose and eyes, it can cause symptoms that resemble asthma, such as a persistent cough and shortness of breath. However, hay fever symptoms are typically triggered by exposure to allergens like pollen, pet dander, or dust mites.
Respiratory Infections
Certain respiratory infections, such as bronchiolitis or respiratory syncytial virus (RSV), can mimic asthma symptoms in young children. These infections often cause wheezing and difficulty breathing, just like asthma. However, unlike asthma, respiratory infections are usually temporary and will resolve once the infection clears.
Medical and Family History
Importance of medical and family history
When evaluating respiratory conditions, including asthma, medical and family history play a crucial role. Certain risk factors, such as a family history of asthma or allergies, can increase the likelihood of developing asthma. Additionally, understanding a patient’s overall medical history can help identify potential triggers, such as exposure to environmental toxins or a history of respiratory infections.
Specific questions to ask
During a medical evaluation, healthcare professionals may ask specific questions to help differentiate between asthma and other respiratory conditions. These questions may include:
- Do you have a family history of asthma or allergies?
- Have you had respiratory infections or bronchitis in the past?
- Do you experience symptoms in specific environments or after exposure to certain triggers?
- What medications or treatments have you tried in the past, and how did you respond to them?
These questions aid in gathering important information that can guide the diagnostic process and inform the appropriate treatment plan.
Physical Examination
Overview of a physical examination
During a physical examination, a healthcare professional will evaluate various aspects of your health to assess for any signs or symptoms indicative of respiratory conditions. They will listen to your breathing using a stethoscope and check for any abnormal lung sounds, such as wheezing or crackles. Additionally, they may examine your nose, throat, and chest to identify any physical abnormalities or signs of inflammation.
Signs that may indicate asthma or other respiratory conditions
During a physical examination, certain signs may point towards asthma or other respiratory conditions. These signs can include:
- Wheezing: A whistling sound heard during breathing.
- Cyanosis: Bluish discoloration of the lips or skin due to lack of oxygen.
- Abnormal lung sounds: Crackles, wheezes, or decreased breath sounds.
- Nasal congestion or discharge: Indicative of nasal inflammation or chronic rhinitis.
However, it’s important to note that a physical examination alone cannot definitively diagnose asthma or rule out other respiratory conditions. Additional tests and assessments are often necessary to establish an accurate diagnosis.
Pulmonary Function Tests
Spirometry
Spirometry is a common pulmonary function test used to measure how well the lungs function. It assesses lung capacity, airflow, and the presence of any obstruction. Spirometry measures the volume of air you can forcefully exhale in one second (FEV1) and the total volume exhaled (forced vital capacity or FVC). This test is helpful in diagnosing and monitoring asthma, as it can identify any airflow limitation.
Peak Flow Meter
A peak flow meter is a portable device used to measure how fast you can expel air from your lungs. It is particularly useful for individuals with asthma as it can provide an objective measure of lung function. By regularly using a peak flow meter, you can track changes in your lung function and identify any patterns or triggers that may provoke asthma symptoms.
Methacholine Challenge Test
The methacholine challenge test is used to assess bronchial hyperresponsiveness, a characteristic feature of asthma. During this test, the patient inhales increasing concentrations of methacholine, a substance that causes the airways to constrict. If the airways constrict significantly, it indicates a positive result, suggesting a diagnosis of asthma.
Fractional Exhaled Nitric Oxide (FeNO) Test
The FeNO test measures the level of nitric oxide in your breath, which can be elevated in individuals with asthma. Nitric oxide is produced by inflamed airways, and elevated levels may indicate ongoing airway inflammation. This test can help confirm an asthma diagnosis and monitor the effectiveness of treatment over time.
Chest X-rays and Imaging Tests
Chest X-rays
Chest X-rays are imaging tests that provide detailed images of the lungs and surrounding structures. While they are not typically used to diagnose asthma directly, they can help rule out other conditions, such as pneumonia or lung masses, that can present with similar symptoms. Chest X-rays can also reveal any structural abnormalities or signs of infection that may contribute to respiratory symptoms.
Computed Tomography (CT) Scan
A CT scan provides a more detailed view of the lungs and can help identify and evaluate structural abnormalities or lung diseases. It can be particularly useful in cases where chest X-rays do not provide enough information, or when there is a suspicion of more complex respiratory conditions.
Magnetic Resonance Imaging (MRI)
While not commonly used for routine evaluation of asthma, an MRI may be ordered in specific cases where further evaluation of the lungs or surrounding structures is needed. MRI scans use powerful magnets and radio waves to create detailed images, helping to identify any abnormalities that might be causing respiratory symptoms.
Lung Function Studies
Arterial Blood Gas (ABG) Test
An arterial blood gas (ABG) test is used to assess the levels of oxygen and carbon dioxide in your blood, as well as the pH level. It is typically done by taking a sample of blood from an artery, usually in the wrist. ABG tests are helpful in evaluating lung function and determining if there is an adequate exchange of gases in the lungs.
Pulse Oximetry
Pulse oximetry is a non-invasive test that measures the oxygen saturation levels in your blood. It involves a small device called a pulse oximeter, which is placed on your finger or earlobe. The pulse oximeter uses light absorption to determine the amount of oxygen your red blood cells are carrying. This test can provide valuable information about your lung function and the efficiency of gas exchange in your bloodstream.
Allergy Testing
Skin Prick Test
A skin prick test, also known as a puncture or scratch test, is the most common method used to diagnose allergies. It involves placing small amounts of various allergens on your skin, usually on your forearm or back, and then pricking or scratching the surface of the skin to allow the allergens to enter. If you are allergic to a particular substance, you will develop a small raised bump on the skin at the site of the allergen.
Blood Test (RAST or ELISA)
Blood tests, such as the radioallergosorbent test (RAST) or enzyme-linked immunosorbent assay (ELISA), can also be used to detect specific allergies. A blood sample is taken and tested for specific antibodies that are produced when the immune system encounters an allergen. These tests can help identify potential triggers for asthma symptoms, such as allergens like pollen, pet dander, or dust mites.
Patch Test
Patch testing is primarily used to diagnose contact dermatitis, a condition characterized by a skin reaction upon contact with certain substances. However, in some cases, patch testing may be beneficial for individuals with suspected respiratory allergies. Tiny amounts of potential allergens are applied to patches and placed on the skin for a specific period. If a reaction occurs, it suggests sensitization to that allergen.
Differential Diagnosis
Process of differential diagnosis
Differential diagnosis is the process of distinguishing one condition from another that may have similar symptoms. When it comes to respiratory conditions, distinguishing asthma from other diseases is important to ensure appropriate treatment. This process involves a thorough evaluation of symptoms, medical history, physical examination, and the results of various diagnostic tests.
Importance of ruling out other conditions
Ruling out other respiratory conditions is crucial to ensure accurate diagnosis and appropriate treatment. Different conditions require different management strategies, and misdiagnosing asthma can lead to ineffective or potentially harmful treatments. By carefully considering the patient’s symptoms, medical history, and test results, healthcare professionals can confidently differentiate between asthma and alternative respiratory conditions.
Treatment Options
Bronchodilators
Bronchodilators are medications that help relax and open up the airways, making it easier to breathe. They are a common treatment for asthma and can provide quick relief from symptoms such as wheezing and shortness of breath. Bronchodilators come in various forms, including inhalers and nebulizers, and may be prescribed for both acute symptom relief and long-term control.
Inhaled Corticosteroids
Inhaled corticosteroids are anti-inflammatory medications that reduce inflammation and swelling in the airways. They are often used as a long-term treatment option for asthma management to prevent symptoms and decrease the frequency of asthma attacks. These medications are typically taken daily and help to control airway inflammation, reducing the risk of exacerbations.
Immunotherapy
Immunotherapy, also known as allergy shots, is a treatment option for individuals with asthma triggered by specific allergens. It involves receiving regular injections of small amounts of the allergen to which you are allergic. Over time, the immune system becomes desensitized to the allergen, reducing the severity of allergy symptoms, including asthma.
Lifestyle and Environmental Changes
Making certain lifestyle and environmental changes can also help manage asthma symptoms. Some strategies include:
- Avoiding triggers: Identify and avoid exposure to allergens or irritants that worsen your asthma symptoms, such as smoke, pollen, or pet dander.
- Using a humidifier or dehumidifier: Maintaining optimal humidity levels in your home can help prevent respiratory symptoms.
- Regular exercise: Staying physically active can improve lung function and overall respiratory health. However, it’s essential to consult with your healthcare provider to develop an exercise plan that is appropriate for your asthma condition.
- Proper asthma management: Follow your healthcare provider’s prescribed treatment plan, including taking medications as directed, tracking symptoms, and attending regular check-ups.
By implementing these lifestyle changes and working closely with your healthcare team, you can effectively manage your asthma and improve your overall quality of life.
In conclusion, differentiating between asthma and other respiratory conditions can be challenging due to overlapping symptoms. Medical and family history, physical examination, and various diagnostic tests are essential in accurately diagnosing asthma and ruling out similar conditions. Treatment options for asthma include bronchodilators, inhaled corticosteroids, immunotherapy, and lifestyle/environmental changes. It is essential to consult with a healthcare professional for proper evaluation, diagnosis, and treatment of respiratory conditions to ensure optimal management and improve quality of life.